Author Jocelyn Davis and organizational psychologist Kelly Kinnebrew are on a mission to build mental health literacy and leadership in the working world. Follow our adventures in this biweekly newsletter and on our website, Mindfalls.org. And please send us your thoughts, questions, and suggestions—we'd love to hear from you!

"Overdiagnosis." Right now, it's the loudest criticism directed at the mental healthcare system. "We're medicalizing normal human emotions," the critics say. "Every kid is in therapy. Doctors hand out meds like candy. If you're feeling sad, worried, or distracted, there's a label and a drug for that. It's actually fashionable to have a mental illness." In the old days, they say, people were resilient. Things were better then.
And yet ... this past summer, when we interviewed 23 people who'd navigated a mental collapse, we heard tale after tale of underdiagnosis with a side of dismissiveness: "The lab tests say you're fine." "Have you tried meditation? Or yoga?" "Still getting up at the crack of noon, I see." And our personal favorite, from a distinguished neurologist to a woman who'd been confined in a psych ward and was seeking explanations: "Pfft. You just got in a funk."
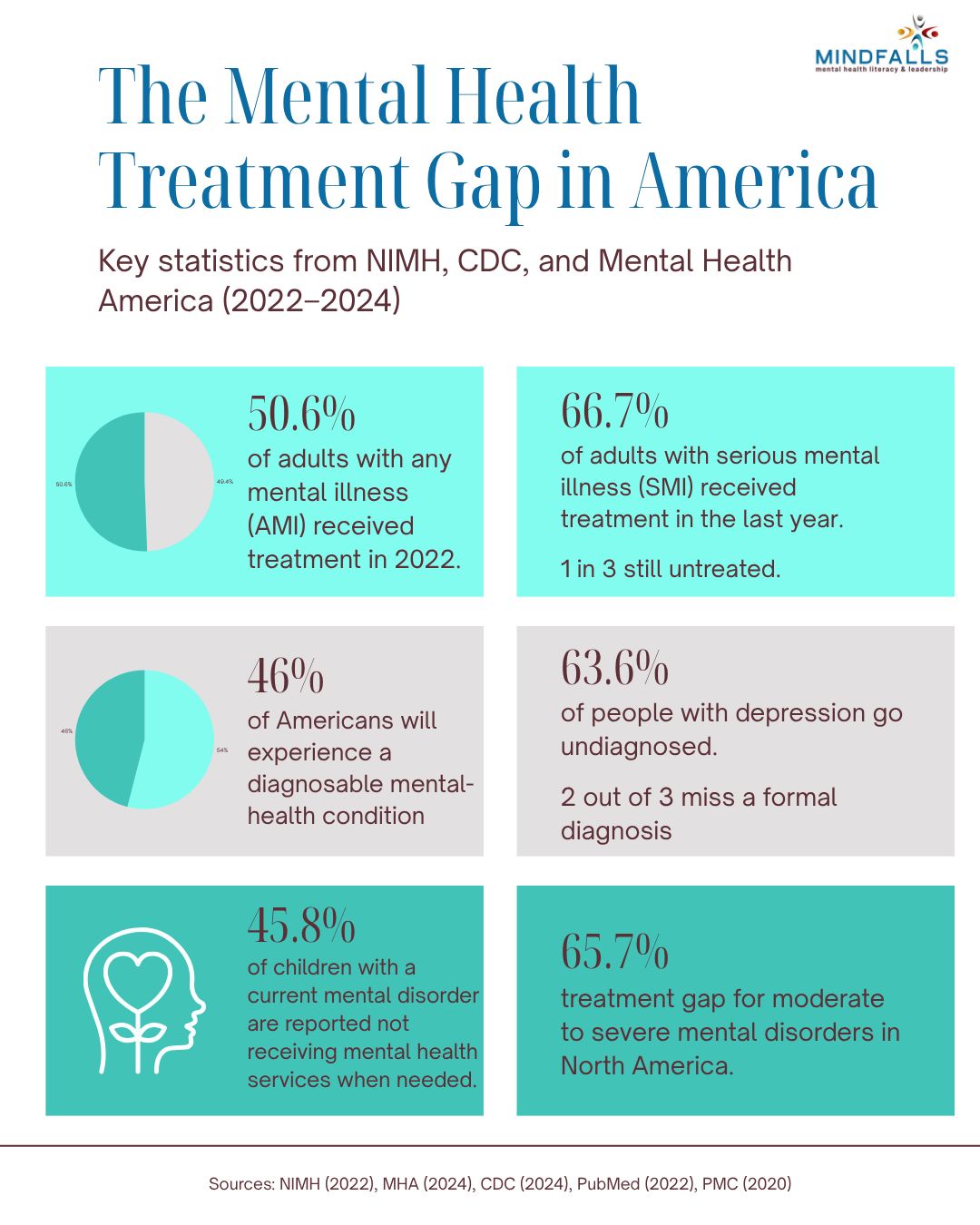
Maybe over vs. under isn't the right frame. Surely what we want, when it comes to mental health, isn't less diagnosis or more diagnosis, but accurate diagnosis and effective help for those suffering from serious mental dysfunction. In this inaugural issue, we'll look at how to stop fixating on a false dichotomy and start taking a broader view of the phenomenon we call mindfalls.



by Jocelyn Davis
What’s the bigger problem in mental health today: overdiagnosis or underdiagnosis?
On the one hand, we have authors such as Abigail Shrier (Bad Therapy) and Allen Frances (Saving Normal) claiming we’re all being shoved into therapy, slapped with labels, and prescribed meds for complaints that, in the old days, would have been considered ordinary aspects of the human condition and treated with a prescription to suck it up. On the other hand, we have organizations like the CDC pointing to alarming increases in rates of mental illness, substance abuse, and suicidality to support their view that we aren’t giving enough attention to very real, often life-threatening disorders.
As usual, the truth lies in the middle. Whether your mental health challenges are met with suffocating over-analysis or callous dismissiveness—or a weird combination of both—depends on your age, sex, cultural background, personality, and a host of other factors. The trick is to do what you can to elicit “Goldilocks help”: not underdone, not overdone, but just right for you.

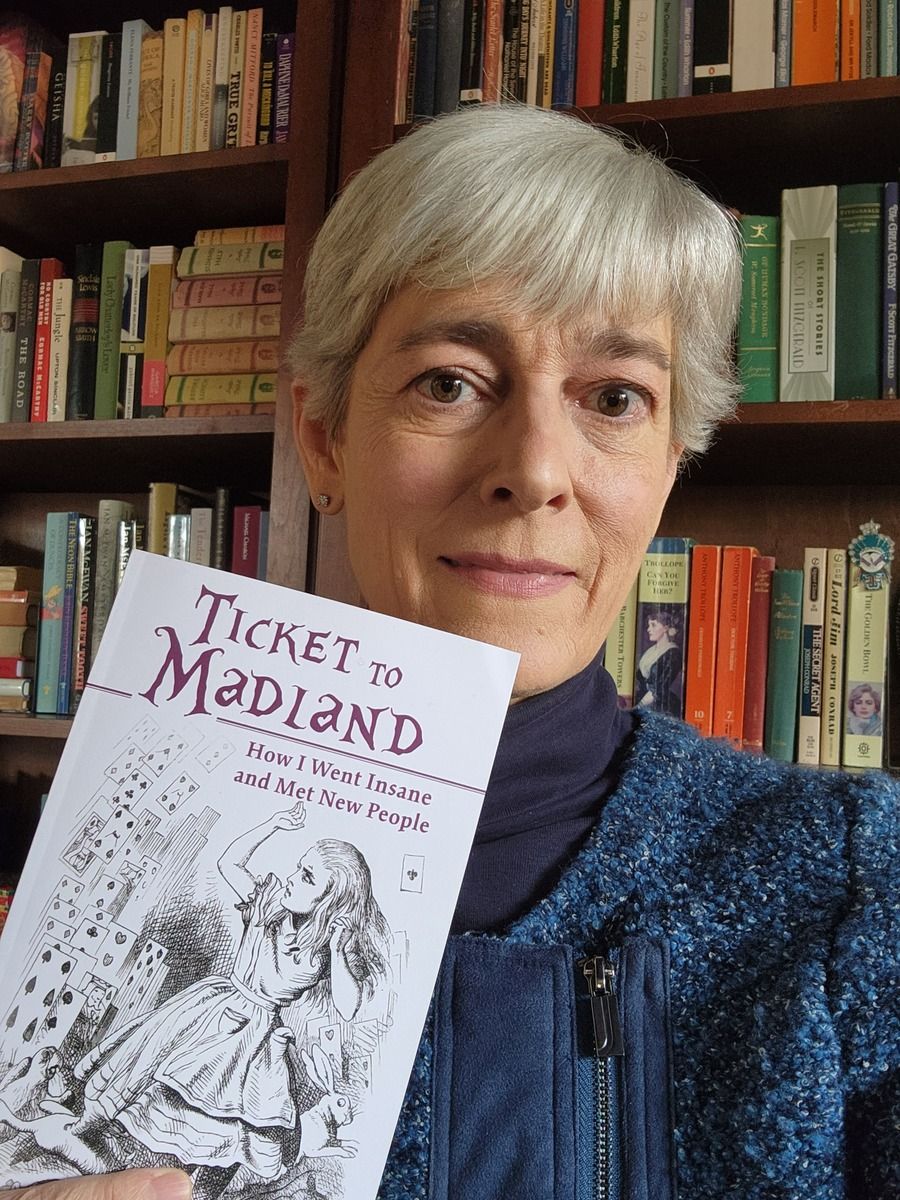
TICKET TO MADLAND: BOOK EXCERPT
Ticket to Madland is the harrowing yet humorous story of my trek through a bizarre brain-body illness, culminating with two weeks in a locked psych ward. “Reads like a medical thriller,” says one reviewer. (Spoiler: I recovered.)
The scene below takes place in October 2020: nine months into the Covid pandemic, eleven weeks into my ordeal. I’ve secured an appointment with an eminent neurologist who is going to underdiagnose me. Although he was kind of a jerk, I must admit that my approach didn’t help. I wish I could go back and share these tips with my former self. –Jocelyn D.
***
“I want you to remember these three words: green, Denver, horse. Repeat them back to me.”
“Green, Denver, horse.”
“Good. Now, spell ‘world’ backward.”
“D … um … d, l …” Perched on the end of the exam table in Dr. Andersen’s office deep in the labyrinth of Mountain Medical Center, I struggled to picture the word world backward. World is w, o, r, l, d, now reverse it, c’mon, it’s only one syllable. “D, l … um … r, o, w.”
“Now repeat the three words I asked you to remember.”
“Green, Denver, horse.” (Did I pass? Did I pass?)
Dr. Ortega, upon prescribing the Lexapro, had given me names of a few neurologists. Covid was raging in Santa Fe, making it nearly impossible to get in to see any doctor, let alone a specialist, but when I called Mountain Medical to inquire about Dr. Andersen, they astonished me by saying he had an opening the next day at ten a.m. I booked the appointment.
The facility was fancier than most, with an airy, high-ceilinged lobby guarded by receptionists in germ-safe glass booths and furnished with purple-and-green striped couches that almost matched my purple blazer and green glass earrings. (Well-groomed!) Although the buzzing anxiety was now near-constant, I was still able to hide it well enough, and when the ponytailed nurse came to the waiting area to fetch me, I rose, dusted off my purple shoulders, adjusted my mask, and followed her into the labyrinth chatting cordially. The interior was 21st century high-tech, brimming with white, chrome, and beige, like an IKEA.
Nurse Ponytail spent a good fifteen minutes recording my history and symptoms. She also asked me a set of questions about depression. I didn’t like having to answer eight of the ten with “yes” or “almost always,” but I was determined to be truthful. One question to which I answered “no” was Do you have a suicide plan? This, I would later learn, is the main question the pros use in order to gauge depression’s severity: if suicidal ideation is a red flag, having a plan is thought to be a much redder flag, a sign you’re much closer to doing the deed. The other outlier question was Do you feel guilty about how your depression is affecting those close to you? I thought about that for a moment: Did I feel guilty? “No, I can’t say I feel guilty,” I said as Nurse Ponytail typed away, “but I know this whole situation is making things very tough on my husband. Really, I just want to get better.” She thanked me and said the doctor would be in shortly.

10 Mental Health Must-Haves As Workplace Anxiety Skyrockets - Mental health has become a central concern in today’s workplaces, with rising rates of stress, loneliness, and burnout underscoring the need for proactive employer action. Building mental health literacy through learning and development (L&D) initiatives empowers employees and leaders to recognize distress, seek support, and foster open dialogue around well-being. By embedding mental health education, empathy-based leadership training, and supportive organizational practices, companies can create resilient, connected, and thriving workplace cultures.
Cultivating Mental Health Literacy: Empowering the Workplace Through Education and Support - As workplace anxiety and burnout reach record highs—affecting 66% of U.S. workers in 2025—experts are urging both employees and employers to prioritize mental health as essential to safety and performance. Employees are encouraged to create personal “work care plans” that include practices such as meditation, exercise, proper sleep, and social connection to counter toxic work environments. Meanwhile, organizations must address systemic issues by removing toxic employees and managers, providing growth opportunities, and expanding mental health benefits to build healthier, more sustainable workplaces.
Over a Billion People Living With Mental Health Conditions – Services Require Urgent Scale-Up - More than 1 billion people are living with mental health disorders, according to new data released by the World Health Organization (WHO), with conditions such as anxiety and depression inflicting immense human and economic tolls. While many countries have bolstered their mental health policies and programmes, greater investment and action are needed globally to scale up services to protect and promote people’s mental health.
State of the World’s Emotional Health 2025 - The world is on an emotional edge. Gallup World Poll data show that in 2024, 39% of adults worldwide reported worrying for much of the previous day, and more than a third said they felt stressed. Compared with a decade ago, hundreds of millions more people now experience these emotions.

Common Mental Health Issues That Are Frequently Misdiagnosed - Most people with substance use disorders have one or more co-occurring mental health issues. Typically, the mental health issue comes first and drives addictive behavior, but drugs and alcohol also make mental health issues worse. Accurately diagnosing and effectively treating any co-occurring mental health issues is one of the most important parts of a strong recovery from addiction. Unfortunately, neither diagnosis nor treatment is as straightforward as one would hope.
An Overdiagnosis Epidemic Is Harming Patients’ Mental Health | WIRED -Diagnosing patients when there aren’t effective treatments to give them can make their symptoms worse, argues neurologist Suzanne O’Sullivan.
Adult ADHD: Overdiagnosed? Or finally getting the attention it deserves? | AAMC - 15 million U.S. adults say they have a diagnosis of attention deficit hyperactivity disorder. But some experts worry that ADHD can be overhyped and that too few doctors are prepared to treat a condition that was long considered an issue only for kids.
The Mindfalls newsletter is for informational purposes and is not a substitute for professional help. If you are having a mental health crisis, call or text the 988 Suicide & Crisis Lifeline, reach out to your doctor, or go to the nearest emergency room.