What’s the bigger problem in mental health today: overdiagnosis or underdiagnosis?
On the one hand, we have authors such as Abigail Shrier (Bad Therapy) and Allen Frances (Saving Normal) claiming we’re all being shoved into therapy, slapped with labels, and prescribed meds for complaints that, in the old days, would have been considered ordinary aspects of the human condition and treated with a prescription to suck it up. On the other hand, we have organizations like the CDC pointing to alarming increases in rates of mental illness, substance abuse, and suicidality to support their view that we aren’t giving enough attention to very real, often life-threatening disorders.
As usual, the truth lies in the middle. Whether your mental health challenges are met with suffocating over-analysis or callous dismissiveness—or a weird combination of both—depends on your age, sex, cultural background, personality, and a host of other factors. The trick is to do what you can to elicit “Goldilocks help”: not underdone, not overdone, but just right for you.
Three Tips to Avoid Underdiagnosis
If you’re over 45, know that you were likely taught to be invulnerable.
“Get over it.” That was your parents’ reaction when you expressed anger, sadness, or any other unpleasant emotion. As a result, you developed resilience, and it has served you well. But you also probably developed a level of self-sufficiency that’s unhelpful when you’re truly struggling. If you’re a boomer or Gen X, mental toughness can be a liability. Don’t let a hard shell keep you from revealing what’s going on, don’t mistake burnout for a strong work ethic, and don’t resist a mental health diagnosis out of fear or shame.
Don’t just say how you feel; say how you’re (not) functioning.
When a doctor gives you that “all in your head” look, it feels like pure arrogance. Consider, though, that medical pros are trained to look for observable, measurable problems they can treat. So, help them see the problem: along with feelings, describe specific behaviors and outcomes. For example: “I’m sleeping 16 hours a day and missing work.” “I’m so irritable, my partner doesn’t want to be around me.” “I can’t hold my grandbaby because I’m afraid I’ll drop her.”
Ask the doctor about your screening results.
Most mental health appointments begin with a nurse or tech asking you nine or ten questions along the lines of “How often do you feel depressed/anxious/suicidal?” Your answers yield a numerical score. You’d think a doctor would check the results before seeing you, but because of time pressure to get to the examination, many don’t. Be sure to ask, “What is my mental health screening score? What does that score mean?” Again, being specific helps you get through.
Three Tips to Avoid Overdiagnosis
If you’re under 35, know that you were likely taught to overthink and overshare.
Starting in the late 80s, attitudes toward emotional distress shifted from “suck it up” to “spew it out.” Chances are you learned young that the way to handle uncomfortable feelings is to reflect, analyze, and share, share, share. But this sort of rumination can backfire; the human psyche isn’t designed to focus on itself all day. Take courage in the truth that life comes with hardship and we are equipped to cope. Mostly, our minds are like Weebles: they wobble, but they don’t fall down.
Be skeptical of any label you’re given after one brief session.
The average appointment with a PCP lasts 15 minutes; with a therapist, 45 minutes. No mental disorder can be conclusively diagnosed in that brief time. This isn’t to say you shouldn’t trust your doctor; you should, however, take any diagnostic label under advisement. Get a second opinion. Get a third opinion. And even if you think you have the answer, never let go of a curious attitude that keeps you asking questions about your health and treatments.
Act on advice to do ordinary healthy stuff.
“Get more sleep.” “Eat right.” “Go for a walk.” The well-meaning suggestions can be infuriating when you’re struggling just to function. And yes, some of us need medication to get to a place where we can sleep, eat, and walk. That said, it’s incontrovertible that rest, diet, and exercise make a huge difference to our mental health. Staring at screens for most of the day is bad for body and mind. Sunshine lifts spirits. Good habits take a while to build, but they pay big dividends.
Stuck in the Middle
What if you’re an older millennial, aged 35 to 45? Depending on your upbringing and temperament, you may find yourself being undertreated or overtreated. Fortunately, the tips above are all compatible. Your main challenge may be to discern whether you’re dealing with normal emotional reactions to a particular situation or with an entrenched disorder that needs professional help. If you need counsel, it’s never a mistake to reach out: to a family member, friend, therapist, or doctor. If the conversation feels wrong, trust your gut and try someone else.
Bottom line: Goldilocks help—not underdone, not overdone, but just right—is out there. You’ll know it when you see it.
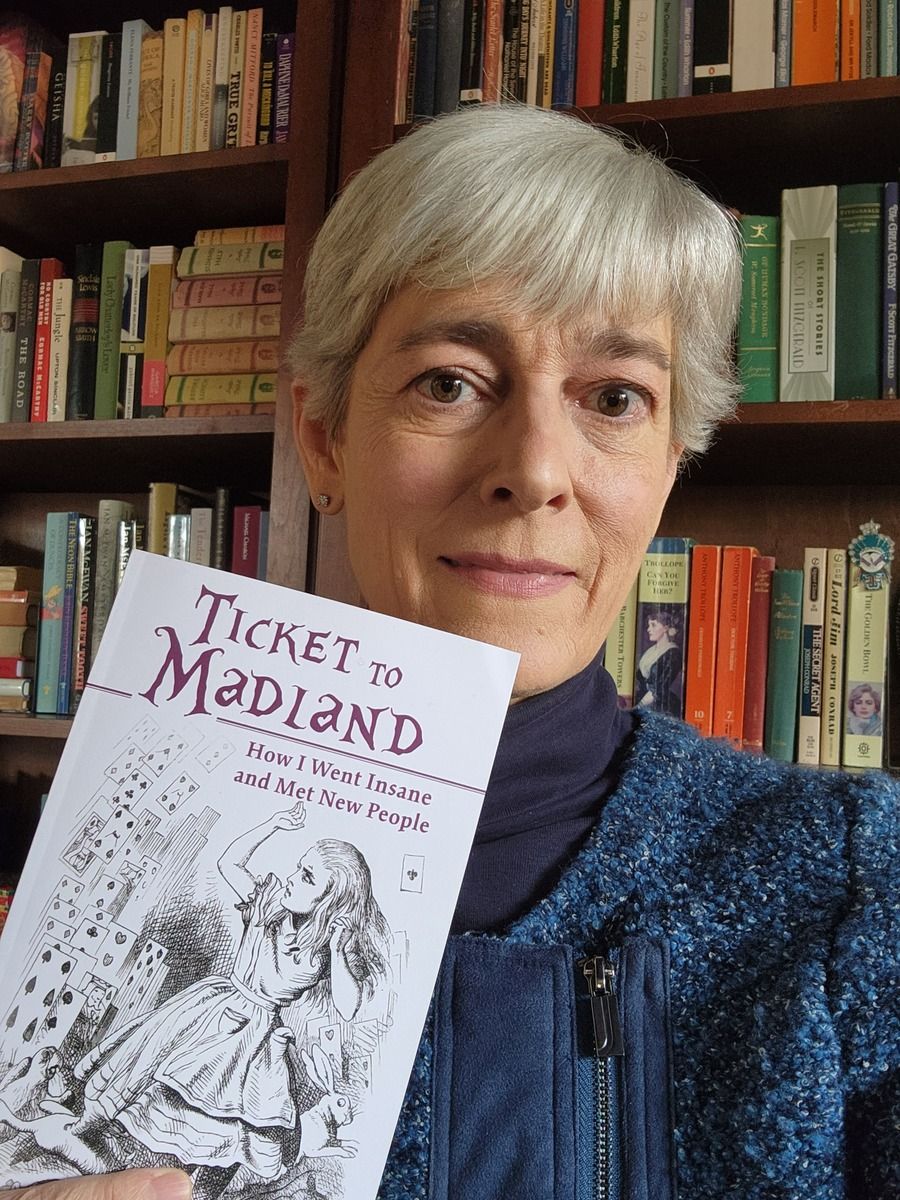
Jocelyn Davis writes books about leadership, folklore, and mental health. Learn more at JocelynRDavis.com.