First aid for mental health is becoming quite a thing. Search "mental health first aid certification" and up will pop scores of organizations like this one, all promising to teach you how to recognize signs of a "mental health or substance use challenge" then offer the "first level of support."
We see the appeal of these programs. After all, mental emergencies are even scarier than physical ones. With a heart attack or a head wound, you at least have a sense of what's happening and what to do about it: call 911, perform CPR, stop the bleeding. But if your colleague or friend is just, like, acting weird ... What do you do? Should you even get involved? What if you make it worse?
So it's a comforting idea--first aid for the mind, as for the body. If such training builds confidence in a crisis, we're all for it. But anyone who's navigated a serious mental breakdown will tell you: It's the second aid that counts. And it's not just professionals who can and should provide it.
What does (actually aidful) second aid for mental health look like? Find out in this latest issue of Mindfalls.




by Jocelyn Davis
What can you do for someone who’s having a mental breakdown? Recognize the signs. Make them comfortable. Call the HR rep, a family member, or emergency services to come handle the situation. (Extra step if you’re British: Make tea.)
That’s mental health first aid: the equivalent of getting a blanket and summoning an ambulance for Dad’s slip-and-fall in the driveway. Anything beyond these basic measures, you might think, is for the professionals to worry about.
Actually, there’s a lot more we can do.
Yes, professional help is best left to professionals, but in matters of mental health—with its complex mix of physical, emotional, social, and even spiritual elements—support from family and friends can be crucial. In my own journey through Madland, homegrown second aid was just as important to recovery as anything I got in a medical office.
Jocelyn Davis writes books about leadership, history and literature, and mental health. Learn more at JocelynRDavis.com.

On Being There for Someone Spiraling
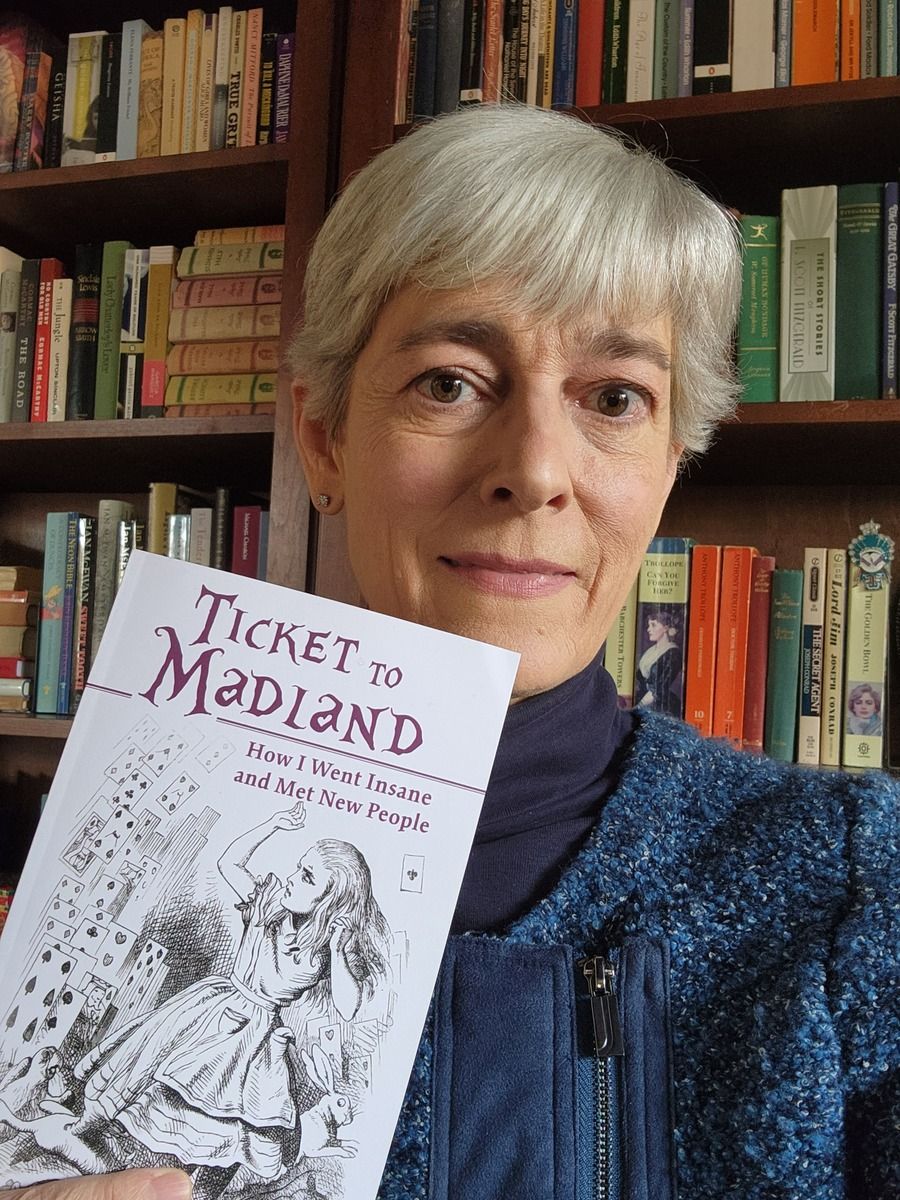
Ticket to Madland is the fearsome, funny story of my four-month journey through a mysterious mind-body illness, which took me through doctor and therapist offices, a rehab center, and a locked psych ward. (Spoiler: I recovered.)
In this excerpt, I reflect on the friends, family, and professionals who were trying to help as I slid down the hole in late October 2020. I called them my defense team, but as you’ll see, they were really something else.
***
My entire defense team meant well; they tried their best. Yet I remained in the prisoner’s dock, looking at them looking at me, a wall of glass between us, the floor under my feet bumping down, down, like a janky elevator, taking me farther from aid and nearer to the executioner’s block. What would I say to them now, other than “Thanks for trying”? What would I say to anyone who wants to defend a friend, patient, or loved one against the brutal encroachments of insanity?
When faced with a mentally ill person, few of us can resist offering advice. We tell the ill one to get outside, stick to a routine, engage in self-care, take supplements, see a therapist, go on vacation, come for a visit, or try Rolfing. We suggest they exercise, journal, breathe, meditate, knit, eat plants, or smoke weed. When we see our advice isn’t landing, most of us know enough to back off: we revert to offering a sympathetic ear, a shoulder to cry on, support as requested. “Talk to me,” we say. “Call me anytime. Let me know how I can help.” And we’re right to say those things. Listening, after all, is what a good friend does. But the critical point we tend to miss is that a person with major depressive disorder isn’t “feeling down.” A person with an anxiety disorder isn’t “experiencing some stress.” A person with obsessive-compulsive disorder isn’t “so anal, ha-ha.” A person with bipolar disorder isn’t “moody.”

With therapy hard to get, people lean on AI for mental health. What are the risks?
When rising costs forced Kristen Johansson out of therapy, she turned to an AI chatbot for daily support, a choice more people are making as human care becomes harder to access. While chatbots can offer convenience and comfort, their growing use raises safety and ethical questions about how they fit alongside real therapists.
Mapping the Sense of What's Going on Inside
Scientists are piecing together how the mind keeps a silent map of everything happening inside us—and what happens when that inner navigation system goes off course.

The ALGEE approach: a short video neatly summarizing the five steps on which many mental health first aid courses are based.
A 24-hour helpline in the UK known as Samaritans helped Sophie Andrews become a survivor of abuse rather than a victim. Now she's paying the favor back as the founder of The Silver Line, a helpline that supports lonely and isolated older people. In a powerful, personal talk, she shares why the simple act of listening (instead of giving advice) is often the best way to help someone in need. This quiet yet gripping TED talk is one of the best we've seen on how nonprofessionals can help those struggling with their mental health.
Finally, here are the slides for Jocelyn's "Let's Talk Mental Illness." This 45-minute interactive talk is a deeper dive into mental health second aid, featuring more stories, more do's and don'ts, plus a bonus anecdote involving raccoons. If you'd like the session online or in-person for your own organization (free with book purchase), drop me a note at [email protected] .
The Mindfalls newsletter is for informational purposes and is not a substitute for professional help. If you are having a mental health crisis, call or text the 988 Suicide & Crisis Lifeline, reach out to your doctor, or go to the nearest emergency room.